Sim Cliff Notes - November 2017
/Every month we summarize our simulation cases. No deep dive here, just the top 5 takeaways from each case. This month we discussed geriatric trauma and penetrating neck injury.
5 Core concepts for Geriatric Trauma
1. Elderly patients' diminished physiologic reserves, co-morbidities, and medications make it more difficult for them to recover from traumatic injury.
2. Every component of the primary survey is different in the elderly.
Airway – Assess for difficult airway predictors and perform 2 person ventilation
- Direct laryngoscopy is more difficult (impaired neck mobility and mouth opening)
- Bag mask ventilation is more difficult (edentulous, facial wasting, stiff lungs/chest wall)
- Breathing - Provide apneic oxygenation during intubation attempt and be prepared for decreased apneic time to intubate
- Elderly desaturate quickly and tolerate hypoxia poorly (reduced central respiratory drive, weakened respiratory muscles, altered chest wall mechanics)
- Elderly are at increased risk of aspiration (blunted ariway reflexes, swallowing disorders, drug effects, delayed gastric emptying)
- Circulation – Be vigilant for shock and consider reducing sedative doses
- Detection of unrecognized shock may be difficult in older trauma patients
- “Normal blood pressures” may be misleading because of the prevalence of preexisting hypertension (hypotension in elderly trauma patient should be considered SBP less than 110 mm Hg)
- Medications such as beta-blockers may blunt tachycardic response
- Elderly have a reduced “maximal heart rate” (“tachycardia” should be considered a heart rate greater than 90)
- Age – related cardiovascular changes, pre-existing disease, and drug interactions enhance hypotensive response to induction and reduced doses (20-30%) of sedatives and hypnotics should be considered
- Detection of unrecognized shock may be difficult in older trauma patients
- Disability – Even minor mechanisms can cause intracranial hemorrhage and cervical spine fractures
- Age related cerebral atrophy stresses and stretches bridging veins, leading to subdural hematomas with minimal shearing stress
- Age related atrophy leads to cerebral contusions due to coup and contracoup impact
- Osteoporosis and other factors make cervical spine fractures 2x as common in elderly, almost half from ground level fall
3. Always consider if a decompensated medical illness (e.g., infection, myocardial infarction) may have precipitated or be exacerbated by their trauma. Have a low threshold for additional testing (eg. ECG).
4. Elder abuse is very under recognized and under reported. Be vigilant for subtle signs of elder abuse and ask your patient (Click here for our recent post on elder abuse)
- The U.S. Department of Justice estimates that 1 in 9 Americans over 60 years old will experience abuse, neglect exploitation this year
- It is estimated that only 1 in 14 elders will report elder abuse
- Victim risk factors include Age > 75, low income, social isolation, minority , financial dependence on caregiver, cognitive impairment
5. The decision to discharge an elderly patient needs to be made with a number of caveats in mind.
- The need for arm slings, crutches, canes and walkers all contribute to gait instability and could lead to a fall without proper social support for patient
- Lower extremity orthopedic injuries confer a particularly high risk for elderly patients, andadmission should be strongly considered
- Any patient who has gait instability, generalized weakness, profound fatigue after their traumatic event, or a recent history of recurrent falls is a poor candidate for discharge
References
1. Brown JB, Gestring ML, Forsythe RM, et al. Systolic blood pressure criteria in the National Trauma Triage Protocol for geriatric trauma: 110 is the new 90. J Trauma Acute Care Surg 2015;78: 352-359.
2. Pontoppidan H, Geffin B, Lowenstein E. Acute respiratory failure in the adult. N Engl J Med 1972; 287(14):690-8.
3. Milzman DP, Rothenhaus TC. Resuscitation of the geriatric patient. Emerge Med Clin North Am 1996: 14(1):233-44
4. Wang H, Coppola M, Robinson RD, et a. Geriatric trauma patients with cervical spine fracture due to ground level fall: Five years experience in a level one trauma center. J Clin Med Res 2013; 5:75-83.
5, McGwin G, Jr., Sims RV, Pulley L, Rosemen JM. Relations among chronic medical conditions, medications, and automobile crashes in the elderly: a population-based case-control study. Am J Epidemiol 2000: 152(5):424-31.
6. McGwin G, Jr., Maclennan PA, Fife JB, Davis GG, Rue LW, 3rd. Preexisting conditions and mortality in older trauma patients. J Trauma 2004; 56 (6):1291-6.
7. American Geriatric Society, British Geriatrics society, and American Academy of Orthopaedic Surgons Panel on falls Prevention. Guidelines for the prevention of falls in older person. J AM Geriatr Soc 2001; 49 (5):664-72.
8. Acierno R, Et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatemnt study. Am J Public Heath. 2010; 100 (2): 2929-297.
5 step approach to Penetrating Neck Injury (PNI)
1. It pays to know your anatomy. . . ask yourself these questions:
Does it violate the platysma?
- The platysma is the anatomic landmark that defines PNI and requires you to do more than simple wound management.
- The platysma is a very thin muscle invested in the subcutaneous fascia (it can be very difficult to identify).
- Gently spread (no probing) the wound edges apart to evaluate if the wound has violated the platysma.
Is the wound in the anterior or posterior triangle?
- ANTERIOR TRIANGLE: Contains more critical structures (Carotid artery, Internal jugular, Vagus nerve, Trachea), more surgically accessible
- POSTERIOR TRIANGLE: Considered a lower risk area (although tragectory of PNI can course back into anterior triangle), contains cervical cord/spine
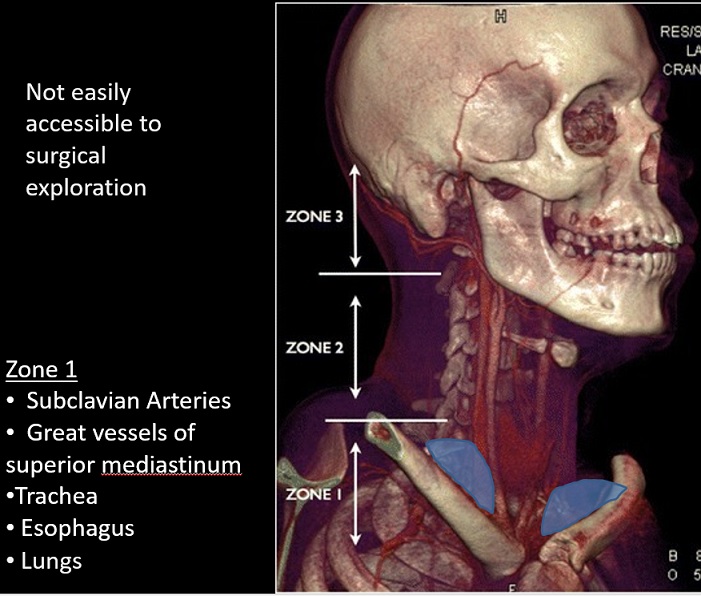
What zone is it in?
- Identifying the zone helps anticipate the anatomy that could potentially be injured
Zone designation carries implications for management and prognosis
However, there are problems with the "zone system"
- Refers only to the location of the wound, not the tract of the penetrating object
- Injury to one zone can extend into different zones
- Past algorithms dictated workup/managment based on zone - less so today
- Current PNI diagnosis/treatment algorithms focus on the exam and CTA
2. Perform a targeted history and physical exam, looking for hard signs that mean an immediate trip to the OR (before or after airway management).
- Physical Exam
- Is there an expanding hematoma?
- Bubbling wound?
- Crepitus?
- Stridor?
- Vascular or neurologic deficit?
- Bruit/thrill?
- History
- Are they hoarse?
- Do they have dysphagia?
- Was there pulsatile bleeding prehospital?
- Hemoptysis?
3. Patients with PNI require frequent re-evaluation of their airway - sick trauma patients live or die from problems with their primary survey.
4. If you have to intubate, rapid sequence intubation with video laryngoscopy is probably the best method.
- A large meta-analysis of PNI by Brywczynski et al. helps inform our choice of intubation method (see table 2 below)
- Rapid sequence intubation with direct laryngoscopy has been shown to be successful and effective
- Concern that complete muscle relaxation in a distorted airway could lead to obstruction are unlikely
- Surgical airways are rare (6%)
- Multiple methods have proven successful, however failure rates are higher with nasotracheal intubation
5. The current paradigm for PNI that is stable without hard findings includes CTA of the neck (+/- chest) and selective operation.
References
1. Brywczynski JJ1, Barrett TW, Lyon JA, Cotton BA. Management of penetrating neck injury in the emergency department: a structured literature review. Emerg Med J. 2008 Nov;25(11):711-5. doi: 10.1136/emj.2008.058792.
2. Inaba K. et al. Evaluation of multidetector computed tomography for penetrating neck injury: a prospective multicenter study. Emerg Med J. 2008 Nov;25(11):711-5. doi: 10.1136/emj.2008.058792.
3. Tisherman AT, Bokhari F, Collier B, et al. Clinical practice guidelines: penetrating neck trauma. J Trauma. 2008;64(5):1392-1405.
4. Schaider J, Bailitz J. Neck trauma: don’t put your neck on the line. Emergency Medicine Practice. 2003;5(7):1-28.